Metformin use is associated with lower mortality from bacterial sepsis and improved immunocompetence in Thai diabetes patients with acute melioidosis
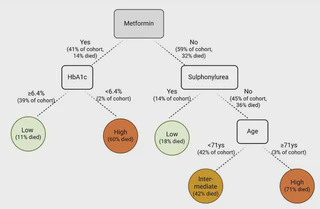 Image credit: Kronsteiner et al.
Image credit: Kronsteiner et al.Background: Diabetes mellitus (DM) is a major risk factor for acquiring infections. Metformin, the first-line treatment for type 2 DM, is associated with beneficial outcome from various infectious diseases. The neglected tropical disease melioidosis has up to 50% in-hospital mortality rate and the highest risk association of DM with any infectious disease (12-fold increased risk). A better understanding of the impact of anti-hyperglycaemic drug treatment on disease outcome is needed.
Methods: We analysed the association of anti-hyperglycaemic treatment on outcome from acute melioidosis in 273 Thai patients with known DM using logistic regression and classification tree modelling while controlling for age, sex, HbA1c and history of renal impairment. Immunological parameters including T-cell and humoral responses to the pathogen as well as cytokine levels in blood were measured in a subset of individuals.
Results: We report higher survival rates in acute melioidosis patients with DM who were taking the glucose-lowering drug metformin prior to infection. Metformin use was associated with a 50% decrease in 28-day mortality whilst renal impairment was associated with a doubling of mortality after adjusting for covariates. Unsupervised classification tree modelling further identified glycaemic control and age as modifying factors of outcome. Furthermore, metformin treatment was associated with greater T-cell responsiveness and the presence of T-cell modulating cytokines.
Conclusions: We provide evidence for a protective effect of metformin in melioidosis and identify HbA1c and age as additional clinically relevant predictors of outcome. Further mechanistic research and randomized controlled trials are required to explore a causal link between metformin and protection from infectious diseases.
Lay summary
Melioidosis is a neglected tropical disease caused by the bacterium Burkholderia pseudomallei, which can be acquired from the environment through contact with soil or water. Type 2 diabetes is a major risk factor in acquiring the infection, though some past studies showed that some diabetes medications prevent deaths from melioidosis. However, although metformin is the most common treatment for diabetes, we don’t know whether it specifically prevents deaths from melioidosis.
To answer this question, we collected data from diabetes patients infected with melioidosis in northeast Thailand, an endemic area for melioidosis. We show that metformin is indeed associated with a decreased risk of death from melioidosis, more so than other diabetes medications. Furthermore, we built a classification tree model, a type of machine learning model, to find the best way to predict whether a patient dies based on their properties. The model identifies metformin usage as the most important factor in helping predict whether a melioidosis patient dies, alongside blood sugar levels and age.
To explain why metformin helps melioidosis patients survive, we investigated the patients’ immune response. We observe that patients on metformin had a greater T-cell response, allowing them to target Burkholderia pseudomallei antigens. These patients also had higher levels of proteins in the blood that allow communication between immune cells to help them defend against bacteria.
Knowing that metformin helps melioidosis patients survive is important because this emphasises why we should help diabetes patients stay on medication as much as possible.
My role
I curated the clinical data to allow the statistical analysis and building of machine learning models.